Causes, Symptoms, Diagnosis, and Management.
Coronary Artery Disease (CAD), also known as Ischemic Heart Disease (IHD), is one of the most significant health challenges globally. It is the leading cause of morbidity and mortality, claiming millions of lives each year. CAD arises from a complex interplay of genetic, lifestyle, and environmental factors, making it a focal point for medical research and public health efforts. This article explores CAD comprehensively, covering its causes, symptoms, diagnostic approaches, and modern treatment options.
Understanding Coronary Artery Disease
What is CAD?

Coronary Artery Disease occurs when the coronary arteries, which supply oxygen-rich blood to the heart muscle, become narrowed or blocked due to plaque formation. This plaque is composed of cholesterol, fatty substances, cellular waste products, and calcium and leads to atherosclerosis.
When the blood supply is restricted, the heart cannot receive enough oxygen, especially during physical exertion or stress, resulting in symptoms such as chest pain (angina) or, in severe cases, a heart attack (myocardial infarction).
Causes and Risk Factors.
- Non-Modifiable Risk Factors.
- Age: The risk of CAD increases with age in men over 45 years of age and in women over 55 years of age.
- Gender: Men are generally at a higher risk, though the risk for women increases post-menopause.
- Genetics: A family history of heart disease significantly elevates the risk of developing CAD.
- Modifiable Risk Factors.
- High Blood Pressure (Hypertension): Persistent high blood pressure strains the heart and damages arteries.
- High Cholesterol Levels:Due to elevated levels of low-density lipoprotein (LDL) cholesterol plaque formation take place.
- Smoking: Tobacco damages the lining of arteries and promotes plaque accumulation.
- Diabetes: Poorly managed diabetes accelerates atherosclerosis by damaging blood vessels.
- Obesity: Excess weight contributes to hypertension, diabetes, and abnormal cholesterol levels.
- Sedentary Lifestyle: Lack of physical activity reduces cardiovascular fitness and contributes to weight gain.
- Unhealthy Diet: Diets rich in trans fats, saturated fats, and sodium can worsen cholesterol levels and blood pressure.
3. Emerging Risk Factors.
- Chronic Stress: Prolonged stress can raise blood pressure and lead to unhealthy behaviors like overeating or smoking.
- Sleep Disorders: Conditions like sleep apnea have been linked to increased CAD risk.
- Air Pollution: Exposure to fine particulate matter has been shown to contribute to cardiovascular problems.
Symptoms of Coronary Artery Disease.
The symptoms of CAD vary depending on the severity of arterial blockage. Some individuals may remain asymptomatic until a major cardiac event occurs.
Common Symptoms.

- Angina: Chest pain or discomfort, often described as pressure, squeezing, or tightness radiating till lower jaw
- Shortness of Breath: Difficulty in breathing that is arising especially during physical exertion.
- Fatigue: Persistent tiredness due to inadequate blood supply to the heart.
- Heart Palpitations: An irregular or fast heartbeat.
Advanced Symptoms.
- Heart Attack: Symptoms include intense chest pain radiating to the arm, neck, or jaw, sweating, nausea, and dizziness.
- Heart Failure: Symptoms include leg swelling (edema), severe shortness of breath, and fluid retention.
Diagnosis of Coronary Artery Disease.
Early and accurate diagnosis are essential to prevent from complications. Physicians for the evaluation of CAD used clinical history, physical examination, and diagnostic tests.
- Clinical Evaluation.
- Medical History: In this method we do assessment of symptoms,take family history, and asking about risk factors from patients.
- Physical Examination: Checking for signs of high blood pressure, cholesterol levels, or other contributing conditions.
- Diagnostic Tests.
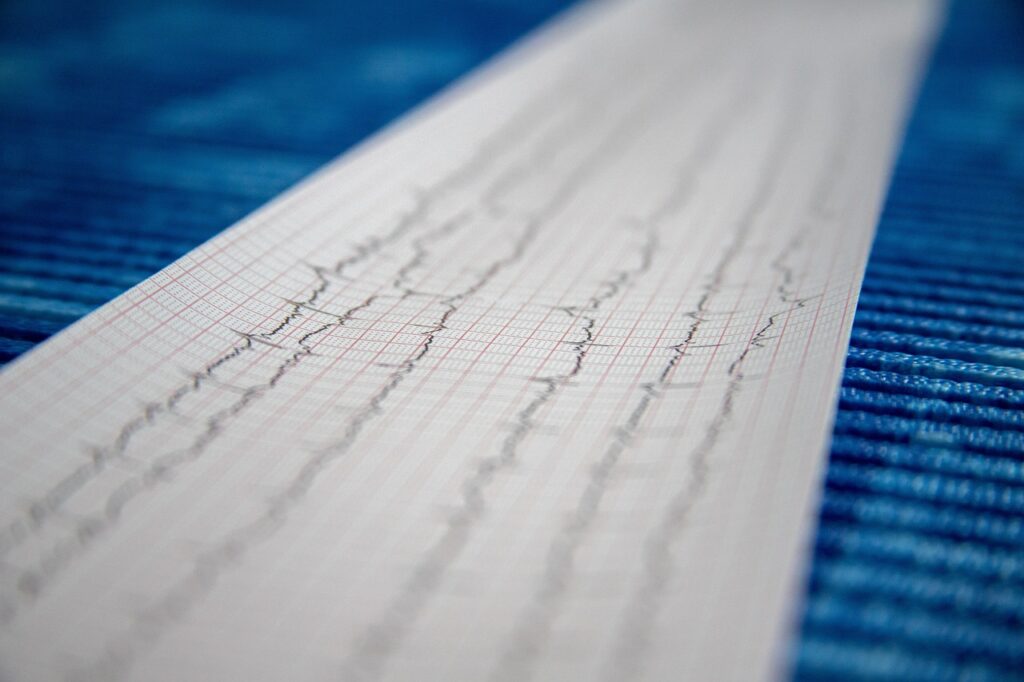
- Electrocardiogram (ECG): It records heart’s electrical activity to detect abnormalities.
- Echocardiogram: This method visualize the heart’s structure and functions.
- Stress Test: Monitors the heart’s performance under physical or chemical stress.
- Coronary Angiography: An invasive test using dye and X-rays to view blockages in coronary arteries.
- Cardiac CT Scan or MRI: It provides detailed images of the heart and blood vessels.
- Blood Tests: Measures cholesterol levels, blood sugar, and markers of inflammation like C-reactive protein (CRP).
Management and Treatment of Coronary Artery Disease.
The treatment of CAD aims to alleviate symptoms, prevent progression, and reduce the risk of heart attacks or complications. Treatment strategies include lifestyle changes, medications, and interventional procedures.
- Lifestyle Modifications.
- Healthy Diet: Emphasizing fruits, vegetables, whole grains, lean proteins, and reducing saturated fats and sodium.
- Regular Exercise: Patients engage in at least 150 minutes of moderate aerobic activity weekly.
- Smoking Cessation: Quitting smoking improves overall cardiovascular health.
- Weight Management: Healthy weight lowers the risk of hypertension and diabetes.
- Stress Management: Practicing mindfulness, yoga, or meditation to reduce stress levels.
- Medications.
- Statins: Lower LDL cholesterol and stabilize plaques.
- Antiplatelets (e.g., Aspirin): Prevent blood clots that result in heart attacks.
- Beta-Blockers: These medicines reduce heart rate and blood pressure, decreasing the heart’s workload.
- ACE Inhibitors:These inhibitors relaxed blood vessels and in this way decreased blood pressure.
- Nitroglycerin: Relieves angina by dilating blood vessels.
- Interventional Procedures.
- Percutaneous Coronary Intervention (PCI): Also known as angioplasty, this procedure involves inserting a stent to open blocked arteries.
- Coronary Artery Bypass Grafting (CABG): Surgery to bypass blocked arteries using grafts from other parts of the body.
- Emerging Treatments.
- Gene Therapy: This method investigate the ways of development of new blood vessels in the heart.
- Stem Cell Therapy: Investigating the potential for regenerating damaged heart tissue.
- Advanced Imaging Techniques: Enhanced diagnostic tools for earlier detection.
Preventing Coronary Artery Disease.
While some risk factors like age and genetics are uncontrollable, many preventive measures can significantly reduce the likelihood of developing CAD.
Primary Prevention.
- Adopting a heart-healthy lifestyle, including a balanced diet and regular exercise.
- Avoiding tobacco use and limiting alcohol consumption.
- Controlling chronic conditions like diabetes, hypertension, and hyperlipidemia.
Secondary Prevention.
- Following medical advice and adhering to prescribed medications.
- Regular monitoring of blood pressure, cholesterol, and glucose levels.
- Undergoing routine health screenings, especially for those at higher risk.
The Global Burden and Future Directions.
Coronary Artery Disease remains a public health challenge, especially in low- and middle-income countries experiencing lifestyle transitions. The increasing prevalence underscores the need for accessible healthcare, public awareness campaigns, and investments in preventive strategies.
Future Research Areas.
- Customized medication to tailor treatment based on individual hereditary profiles.
- Advances in wearable technology for continuous heart monitoring.
- Exploring the role of artificial intelligence in diagnosing and managing CAD.
Conclusion.
Coronary Artery Disease is a life-threatening condition, but it is also largely preventable and manageable with early intervention. Awareness of risk factors, symptoms, and treatment options empowers individuals to take proactive steps toward heart health. The ongoing advancements in medical science and technology offer hope for more effective treatments and improved outcomes for millions of people worldwide.
Efforts at the individual, community, and healthcare system levels are essential to combat CAD and ensure a healthier future for all. By prioritizing prevention and early intervention, we can reduce the global burden of this silent killer.



